The estimated reading time for this post is 34 Minutes
Learning Objective: At the conclusion of this continuing medical education activity, the participant will gain an understanding of the pathophysiology of uric acid stone formation and management of patients with uric acid calculi.
Overview/Background
Urolithiasis is a well-known disease that has plagued mankind for thousands of years, with the oldest recorded stone dated to 4800 B.C. [1] It is a universal disease that spares no geographical, cultural, or racial groups. While urolithiasis is a worldwide problem, data shows an increasing prevalence in industrialized nations, such as the United States, now affecting 1 out of 11 individuals. [2] Uric acid is the third most common stone composition, ranking after calcium oxalate and apatite. It is important to have a thorough understanding of the epidemiology and pathophysiology of uric acid nephrolithiasis for the diagnosis, treatment, and prevention of stones in patients with this condition.
Uric acid is present in all body fluids, and the serum level is determined by its rate of synthesis, excretion, and metabolism. In species such as birds and reptiles, uric acid is used as a means of eliminating excess nitrogen. [3, 4] In other lower mammalian species, uric acid is a byproduct of purine metabolism, and is converted to the urine soluble compound, allantoin, by the enzyme uricase. In contrast, humans and some higher primate species have a non-coding uricase gene, resulting in a lack of the uricase enzyme. Therefore, uric acid is the final product of purine metabolism leading to a relative hyperuricemic state, which contributes to pathological processes such as gout and nephrolithiasis.
There are three urinary contributors to the pathophysiology of uric acid stones- persistently low urine pH, low urine volume, and in rare instances hyperuricosuria. Low urinary pH is the main determinant of uric acid stone formation. While hyperuricosuria can contribute to stone formation, elevated urinary uric acid levels can be tolerated in the presence of normal urinary pH without stone formation. Moreover, hyperuricosuria as the sole cause of uric acid nephrolithiasis is considered relatively rare. [6-9] Individuals with obesity, metabolic syndrome, and type 2 diabetes have a much higher incidence of persistently acidic urine and uric acid nephrolithiasis. Insulin resistance is associated with decreased ammonium production in the proximal tubule and decreased in urine pH, creating a favorable environment for uric acid kidney stone formation. [10-12]
Patients with uric acid stones present with signs and symptoms similar to other patients with stones, including pain, hematuria, lower urinary tract symptoms, nausea, and emesis. Low urinary pH and a lower stone attenuation value on computed tomography should lead one to suspect uric acid stone composition. In addition, patients with conditions that promote profound hyperuricosuria, such as myeloproliferative disorders and Lesch-Nyhan syndrome, are also at risk of developing these calculi. Management of uric acid stones is directed at pH manipulation therapy, since uric acid stones dissolve readily in a favorable urinary pH. This is achieved with an alkalinizing agent, such as potassium citrate.
Epidemiology
In the United States, the incidence of nephrolithiasis is estimated to be 0.5% per year and its prevalence is on the rise. [13] In the United States, the prevalence of stone disease has increased from 3.8 % during 1976 to 1980 to 5.2% during 1988 to 1994 to 8.8% during 2007 to 2010. [2, 14] These trends are similar to those of other industrialized nations.
Uric acid stones account for 7-10% of all kidney stones in the United States. One of the earliest stone analyses from the 1960’s showed that 10% of all stones were composed of uric acid. [15] One study showed uric acid comprising 9.7% of stones from patients in the Veterans Administration system. [16, 17] In a retrospective study of 15,000 stones in Newfoundland, uric acid stones accounted for 7% of all stones. [18] A recent analysis of over 43,000 stones by the Mayo Clinic Metals Laboratory showed uric acid comprising 8% of stones. [19]
The frequency of uric acid stones also varies with age, gender, and geographic location. Patients older than 65 years of age are twice as likely to develop uric acid stones when compared to younger patients. [20] One study showed that uric acid was the second most common stone composition after the age of 55 and that men comprised 72% of uric acid stone formers. [19] Countries such as Japan, Israel, and Pakistan have a much higher prevalence of uric acid stones at 16%, 22%, and 28%, respectively. [21-23] While the prevalence of uric acid nephrolithiasis varies globally, the exact cause has not yet been fully elucidated.
Stone formers with obesity, type 2 diabetes mellitus (T2DM), or metabolic syndrome have uric acid stones more frequently when compared to those without these disorders. [24-29] In fact, it was shown that greater body mass index (BMI) and type 2 diabetes mellitus are independent risk factors for uric acid nephrolithiasis. [30]
Purine Metabolism
Amino acids and purines are the two major sources of nitrogenous waste. Amino acid catabolism yields ammonia as a byproduct, which must be excreted or metabolized to glutamine due to its toxicity. Purines are derived from either purine synthesis, increased cell turnover, or dietary sources. Ultimately, all purines are converted into uric acid by the enzyme xanthine oxidase. In humans and higher primates, uric acid is directly excreted, while in other species, it is degraded to urine soluble allantoin by the enzyme uricase.
Glutamine is a substrate for both de novo purine synthesis and the urea cycle and forms a link between amino acid metabolism, purine metabolism, and the urea cycle. While each product (ammonia, urea, and uric acid) is used to eliminate excess nitrogen, each species predominately utilizes one pathway for nitrogen elimination. Fish eliminate nitrogen through passive diffusion of ammonia across their gills, reptiles and birds fecally eliminate uric acid in the crystalline form, and mammals convert ammonia into urea and excrete it in the urine, reserving uric acid primarily for the elimination of purine metabolism byproducts. [3-5]
In humans and higher primates, the uricase gene is silenced by a series of nonsense and frameshift mutations in the promoter and coding regions. Due to their inability to metabolize uric acid, humans have a relative hyperuricemic state, with uric acid concentrations more than 10 times higher than those in other mammals. [31]
At physiologic pH, uric acid exists predominantly as urate, the unbound and ionized form. The production of urate ranges from 300 to 400 mg per day. Although urate production is relatively constant, the overall excretion of urate can vary greatly depending on dietary purine intake. With respect to the uric acid load, the kidneys eliminate two-thirds, the gut eliminates one-third, and a small amount is eliminated in the skin, hair, and nails. [32] In the intestines, bacteria degrade uric acid into carbon dioxide and ammonia. In the kidneys, almost all uric acid is completely filtered by the glomerulus and 90% is reabsorbed in to the blood. Only about 10% of filtered uric acid is excreted in the urine, indicating that the balance between reabsorption and secretion regulates the total amount of uric acid cleared by the kidney. [33, 34] There are three urate transporters in the proximal tubule that regulate serum uric acid: URAT1, GLUT9, and ABCG2. Most of the filtered load of uric acid is reabsorbed in to the blood by the apical urate transporter, URAT1, and the basolateral urate transporter, GLUT9. Urate secretion is regulated by the apical exporter ABCG2, which is considered to play a role in the development of hyperuricemia in patients with gout. [36]
Pathophysiology
Uric acid stone formation requires supersaturation of urinary uric acid. The pathophysiology of uric acid stone formation involves three main components: low urine pH, low urinary volume, and less commonly hyperuricosuria (Appendix A). [37] In uric acid stone forming patients, an overly acidic urine is by far the most important factor, as it increases the urinary content of disassociated uric acid and the tendency for uric acid precipitation. [9]
Answer 1
Low urinary pH
It has been established that low urinary pH is closely associated with uric acid nephrolithiasis, as almost all uric acid stone formers have a persistently low urinary pH despite normal levels of urinary uric acid. [8] When dissolved in water, urate accepts a free proton to become uric acid, Urate + H+ ↔ Uric Acid. Uric acid is a weak acid with a pKa of 5.35 at 37° C. [38] Under normal conditions, the limit of uric acid solubility is approximately 100 mg/L, a level readily exceeded by normal daily uric acid excretion, which averages 500 to 600 mg/L. However, urine pH is a critical factor in determining uric acid solubility. At a pH ≤ 5.5, even modest amounts of uric acid will exceed the solubility limit, whereas at a pH of 6.5, uric acid concentrations can be excessive but remain soluble (Figure 1). This is due to the sharp upswing of the uric acid dissociation curve at a higher pH, ultimately plateauing at a pH of 7.2. Thus, patients with a urine pH ≤ 5.5 and normal uric acid excretion can develop uric acid stones, while those with a normal or higher urinary pH but excessive urate excretion will not.
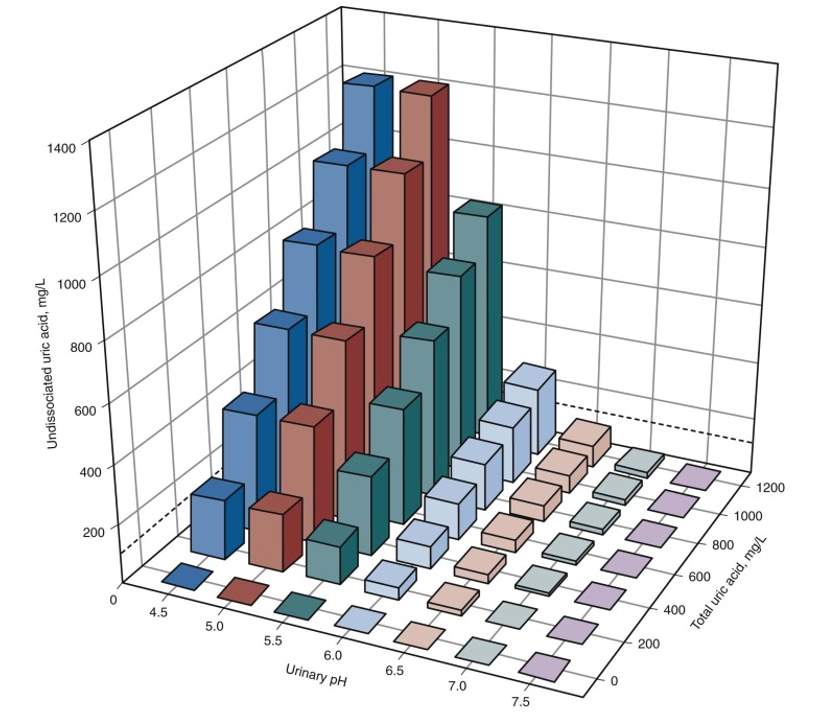
Figure 1. Relationship among undissociated uric acid, total uric acid, and urinary pH. The solubility of uric acid is represented by the dotted line at 100 mg/L. (Reprinted with permission from Dr. Maalouf. Maalouf NM, Cameron MA, Moe OW, et al. Novel insights into the pathogenesis of uric acid nephrolithiasis. Curr Opin Nephrol Hypertens 2004;13:181–9.)
The exact mechanism of persistently acidified urine seen in patients with uric acid stones remains uncertain. Two linked factors appear to promote low urinary pH in this cohort: reduced ammonium (NH4+) excretion resulting in increased net acid excretion. Sakhaee and colleagues compared urinary parameters of acid-base balance in subjects with idiopathic uric acid nephrolithiasis and normal subjects. After equilibration on a controlled diet, not only did uric acid stone formers have persistently acidic urine, but they excreted less of their acid in the form of ammonium, which is thought to be linked to insulin resistance. After an oral acid load with ammonium chloride, these patients further acidified their urine, as they excreted seven times less ammonium than normal subjects. It is proposed that these patients possess a defect in ammonium excretion/generation, leading to a decreased buffering capacity. This results in increased titratable acidity and net acid excretion generating low urinary pH. [9, 26]
Answer 2
Experiments with the Zucker rat, a model for metabolic syndrome, performed by Bobulescu and associates showed that these animals have lower urine pH, lower urinary ammonium excretion and a higher net acid excretion as compared to lean rats. These differences may be related to an increase in renal fat deposition, with fat content being significantly higher in the Zucker rat kidneys. Using an established cell line, this group demonstrated that fat exposure attenuates the generation of ammonium in proximal tubular cells. [39, 40]
These responses have been correlated to the number of components of the metabolic syndrome. Maalouf and others reported that there was a negative correlation between component number, urine pH, and urinary ammonium. [11] A negative correlation between BMI/body weight with urinary pH has been reported by several investigators. In a large group of stone formers, Maalouf and associates reported a significantly negative correlation between urine pH and body weight. [41] Ekeruo and colleagues demonstrated a similar negative correlation between BMI and urine pH in a comparable cohort. [28] Patients with increased BMI are known to have higher levels of visceral obesity and hepatic steatosis, both of which are associated with lower urine pH. [42] Insulin resistance has been found to be significantly correlated with low 24-hour urine pH. Strengthening this association, severe insulin resistance was associated with recurrent uric acid stone formers. [10] Eisner and associates demonstrated that patients with T2DM had more acidic urine. [43] In addition, dyslipidemia has been reported to be associated with low urine pH and higher hemoglobin A1c levels have been demonstrated to be inversely related to urinary pH. [44, 45]
Hyperuricosuria
Dietary intake of animal protein is the most common cause of hyperuricosuria. Rich in purines, animal protein accounts for approximately 30% of urinary uric acid excretion. [46] While hyperuricosuria is a risk factor for uric acid nephrolithiasis, it is rarely the sole cause of stone formation, as acidic urine plays the most important role. Interestingly, patients with a normal urine pH and hyperuricosuria are at risk of forming mixed stones composed of calcium oxalate and urate. If urate concentrations reach high enough levels, uric acid can precipitate. This is thought to cause calcium oxalate crystallization by heterogenous nucleation, or a salting-out phenomenon. [7, 47, 48]
Answer 3
Low urinary volume
Kidney stones form when urine is supersaturated with stone forming solutes. Decreased urinary volume results in increasing concentrations of these solutes. Since the solubility of uric acid is limited, low urine volume and high enough urate concentrations may cause uric acid precipitation. The relationship between kidney stones and low urine volume has been observed, as patients with increased insensible water loss and those in hot, arid, or tropical environments have an increased incidence of stone formation. [49-52]
Etiologies
Gouty diathesis
“Gouty diathesis” is a term coined by Charles Pak to describe patients with uric acid nephrolithiasis, hyperuricemia, decreased fractional excretion of uric acid and low urinary pH, not due to an inborn error of metabolism or secondary causes such as chronic diarrhea, strenuous physical exercise, or excessive intake of animal protein. These patients may or may not have clinical manifestations of gouty arthropathy. The most important feature in these patients is a low urine pH.[9] These patients may also form calcium oxalate or mixed uric acid/calcium stones.
Chronic Diarrhea
Patients with chronic diarrhea are at risk for developing uric acid nephrolithiasis. In inflammatory bowel disease, including ulcerative colitis and Crohn’s disease, the majority of stones contain calcium. However, one third of stones are composed of uric acid, which is higher than the prevalence reported for the general population with uric acid nephrolithiasis. [53-55] In patients with an ileostomy, uric acid stones comprise two-thirds of all stones. [53] In these subjects, acidic urine pH (< 5.5) is commonly encountered as compared to control subjects. [56-58] However, urinary acid excretion has been reported to be normal in this population. [59] In these patients, hypovolemia increases the saturation of stone forming salts, and chronic gastrointestinal loss of bicarbonate with a systemic metabolic acidosis leading to more acidic urine. [56,60]
Insulin Resistance
A definite link insulin resistance and uric acid stone formation has been established. [24-27] Individuals with obesity, metabolic syndrome, and T2DM have a much higher prevalence of uric acid nephrolithiasis at about 30–50% versus 5–8% in the general stone forming population. Many uric acid stone formers exhibit features of the metabolic syndrome, including impaired glucose tolerance or overt diabetes mellitus, truncal obesity, and hyperlipidemia. [24, 27] Insulin resistance is found in over half of subjects with uric acid calculi and diabetic stone formers are almost six-fold more likely to develop uric acid stones than non-diabetic stone formers. [9, 24] Lower urinary pH is associated with insulin insensitivity. [10, 41] This again is due to defective ammonium generation leading to an increase in net acid excretion. This is hypothesized to be caused by renal steatosis and lipotoxicity impacting the proximal tubule.[39, 40]
Diet
Excess animal protein can lead to increased uric acid and calcium excretion, low citrate excretion and reduced urine pH. The aforementioned responses are risk factors for both uric acid and calcium oxalate stones. Individuals who do not have insulin resistance may be able to generate enough ammonium and negate the lowering of urine pH, but those with a combination of a high purine diet and components of the metabolic syndrome have a particularly elevated risk for uric acid nephrolithiasis. [7]
Myeloproliferative Disorders
Patients with myeloproliferative disorders and solid malignancies with a large cell mass often exhibit increased cell turnover with release of nucleic acids and overproduction of uric acid, leading to hyperuricemia and hyperuricosuria. In the setting of chemotherapy initiation, acute tumor lysis can occur, leading to rapid elevation of uric acid levels. This produces a tremendous uric acid load that may result in the generation of uric acid stones and in some uric acid nephropathy. [61] Sickle cell disease, hemolytic anemias, polycythemia vera, and psoriasis are other conditions of high cell turnover that are associated with uric acid nephrolithiasis. [62, 63]
Congenital Disorders
Several congenital diseases are associated with uric acid nephrolithiasis. Some diseases, such as Fanconi syndrome, Hartnup disease, Wilson’s disease, and familial hypouricemic hyperuricosuria (defective uric acid transporter, URAT1) predispose patients to renal wasting of uric acid. Uric acid stones can also occur with inborn errors of metabolism, such as type 1 collagen storage disease, von-Gierke disease and hypoxanthine guanine phosphoribosyl transferase (HGPRT) deficiency, as they cause hyperuricemia and hyperuricosuria. HGPRT deficiency in its most severe form, Lesch-Nyhan syndrome, is characterized by intellectual disability, gout, uric acid nephrolithiasis, and self-mutilation. [64] von-Gierke disease is an autosomal recessive defect in glucose-6-phosphatase and affected patients have hyperuricemia hyperlactatemia, and hypoglycemia. [65]
Evaluation and Diagnosis
Patients may present with a variety of signs and symptoms including pain (abdominal, flank or genital), microscopic or gross hematuria, lower urinary tract symptoms, nausea, and emesis. These findings have both a high sensitivity (80%) and specificity (99%) for detecting nephrolithiasis when patients have a normal appetite, short duration of pain ([66] It is important to obtain a detailed medical history when evaluating patients with suspected uric acid nephrolithiasis. If a patient presents with nephrolithiasis, certain features of metabolic syndrome (obesity, insulin resistance), physicians should have a heightened suspicion for uric acid nephrolithiasis. While calcium oxalate stones are still more common, uric acid stone formation has been shown to be significantly increased in this population. [67]
For evaluation of most patients with acute renal colic, the method of choice is a non-contrast computed tomography (CT) scan of the abdomen and pelvis. A non-contrast CT scan can detect the presence of nephrolithiasis, as it has a 96% sensitivity and a 99% specificity, even for small stones or stones located in the ureter. [68, 69] Uric acid stones have low attenuation values, typically 200-400 Hounsfield units. The proper identification of uric acid stones is improved using a dual source, dual energy CT platform. [70] Another approach for the identification of such stones is a combination of KUB and renal ultrasonography modalities. Uric acid stones are typically radiolucent on plain film imaging. Ultrasonography is a reasonable method for identifying the presence of renal stones, less so for ureteral stones. However, this approach lacks the accuracy, sensitivity, and specificity that can be achieved with CT imaging and may overestimate stone size. [71]
Answer 4, Answer 7
Uric acid stones develop in a more acidic urinary environment. Thus, the presence of low urine pH, typically ≤ 5.5, should raise diagnostic suspicion. Uric acid crystals, which have a diamond, rhombic, or rosette configuration, may be seen on microscopic urinalysis. However, this is not diagnostic for the presence of uric acid stones. [72] Ultimately, a stone analysis is used to confirm the diagnosis. Serum electrolytes, blood urea nitrogen (BUN), creatinine and uric acid should be assessed in patients suspected of having uric acid stones. The serum uric acid is obtained to screen for hyperuricemic states such as gout, and the other parameters to assess renal function.
Management
Some patients that present with acute renal colic due to uric acid nephrolithiasis can be medically managed with adequate pain control and dissolution therapy. Surgical intervention may be necessary in patients who do not respond to dissolution therapy or have complicating features such as severe obstruction, underlying infection, or relentless pain. Surgical stone management is based on stone burden and position. Since uric acids stones are typically radiolucent, shock wave targeting may be challenging. The utilization of ultrasonography or instillation of retrograde, antegrade, or intravenous contrast may be utilized in this setting to direct shock wave energy. [73, 74] Ureteroscopy and percutaneous nephrolithotomy are also effective treatments. Open, laparoscopic, or robotic assisted surgery are rarely necessary.
Long term medical management is directed at correcting the three underlying urinary abnormalities that lead to stone formation: low urine pH, hyperuricosuria, and low urine volume (Appendix B). Urinary pH manipulation therapy is the mainstay for dissolution as well as preventive therapy. This is combined with fluid ingestion for maintenance of adequate urine volume, 2.5 liters or greater for adults. Ideally, 24-hour urine stone risk testing should be obtained to confirm the presence of low pH and for the identification of other stone risk factors that may be contributory. The goal of pH manipulation is to maintain a urinary pH of 6.0 to 7.0. At a pH of 6.0 or greater, uric acid will primarily be in its highly soluble, dissociated form. There is a paucity of studies assessing the effectiveness of oral dissolution therapy. Moran and colleagues treated 11 adult patients harboring large uric acid renal stones with urine pH manipulation and dissolution was achieved in 8 (73%). [75] Elderwy and associates compared dissolution therapy to shockwave lithotripsy in 87 children with radiolucent stones and found that dissolution therapy eliminated the need for shockwave therapy in up to 73% of cases. [76] Dissolution therapyis effective and has been shown to reduce the recurrence of new stone formation from 1.20 to 0.01 stones per year. [77]
Potassium citrate is the first line therapy for uric acid stones with the typical adult dose being 40 to 60 mEq/day. Potassium citrate is generally preferred over sodium alkali salts, as the sodium load in the latter promotes an increase in urine calcium excretion, predisposing the patient to calcium stone formation. [78] In addition, potassium urate is more soluble than sodium urate. However, agents such as sodium bicarbonate or sodium citrate should be considered if the patient does not tolerate the gastrointestinal side effects of potassium citrate or if the patient has impaired renal function and is at risk for hyperkalemia. Baking soda is an alternative source of sodium bicarbonate. Carbonic anhydrase inhibitors, such as acetazolamide, have been used to increase urine pH in those refractory to the aforementioned measures, but are not endorsed for most cases as they induce systemic metabolic acidosis and promote hypocitraturia and hypercalciuria which may lead to calcium phosphate stone formation. [79]
Answer 5
A non-pharmacologic way of increasing urine pH is consumption of fruit and vegetables, especially citrus. Orange juice contains a high content of potassium citrate which can be beneficial for the control of uric acid nephrolithiasis. [80] While lemons contain citric acid, and are generally assumed to deliver an alkali load, some suggest that lemonade is a much less effective therapy for raising the urine pH when compared to orange juice. [81] While fruit juices may be an effective way of alkalinizing the urine to prevent uric acid stones, they are high in calories.
As we have outlined above, almost all uric acid stone formers have some components of the metabolic syndrome and insulin resistance. High calorie fruit juices composed mainly of carbohydrates may be harmful and exacerbate their disease. Emphasis should be placed on weight loss and improvement of insulin resistance, as any weight gain will likely increase the risk for progression of the metabolic syndrome and risk for uric acid stone formation. Patients are also advised to limit consumption of excessive amounts of animal protein, as this has been shown to reduce urine pH and urinary citrate excretion, and augment urinary uric acid and calcium excretion. [82]
Limiting the intake of purine rich foods is also advocated. Adherence to the DASH (Dietary Approach to Stop Hypertension) diet may be a simple way for patients to accomplish these dietary modifications. Ingestion of fruits and vegetables, moderate intake of low-fat dairy products, and low animal protein intake is endorsed with this dietary regimen. Taylor and colleagues demonstrated that patients on a DASH-style diet had a reduced risk for kidney stones and their urine composition exhibited a 16% greater amount of citrate, higher urine potassium, higher urine pH, and lower relative supersaturations of uric acid. [83, 84]
The majority of patients with uric acid stones have low urine pH and do not have hyperuricosuria. Thus, xanthine oxidase inhibitors such as allopurinol and febuxostat should not be routinely offered as a first-line therapy for those with uric acid stones. However, there is a limited cohort of patients with profound hyperuricosuria who may benefit from concomitant therapy with these agents including those with Lesch-Nyhan syndrome, myeloproliferative disorders and tumor lysis syndrome. The development of xanthine stones is a potential side effect of these medications. These stones have similar imaging characteristics to uric acid stones.
Answer 6
Follow-Up
Patients with uric acid stones who are undergoing dissolution therapy need to be observed closely to ensure that stone reduction is occurring. Urine pH should be monitored either with dipstick testing, pH probes, or 24-hour urine testing. Dietary compliance can be assessed with the latter through measurement of urinary sulfate and urea nitrogen which are reflective of animal protein consumption. Urinary potassium is a marker of compliance with ingestion of potassium citrate. Adjustments to the dose of the prescribed alkalinizing agent are made based on urine pH responses. Serum electrolytes should be monitored to assess for hyperkalemia and acid base disturbances. Periodic imaging is obtained to assess for reduction in stone size. This can be done with renal ultrasonography, but CT imaging may be needed to accurately assess response to therapy. A low dose protocol is endorsed when applicable. After successful stone dissolution or stone removal, patients should remain on long-term medical therapy unless the risk factors for stone formation have been reversed.
According to the current AUA guidelines, within six months of the initiation of treatment, clinicians should obtain a single 24-hour urine specimen for stone risk factors to assess response to pharmacologic and/or dietary therapy. [85] Periodic reevaluation of urinary parameters allows the clinician to monitor patient adherence to dietary and drug therapies, and to adjust therapy based on the findings. Clinicians should also periodically obtain follow-up imaging studies to assess for stone growth or new stone formation based on stone activity. [85] In the absence of symptomatic stone episodes, periodic imaging studies can detect failure of therapy and may prompt change in treatment strategy. A one-year imaging interval is recommended for stable patients, but may be adjusted based on stone activity or clinical signs. Again, renal ultrasonography is the ideal modality for long-term follow-up of these patients, but CT imaging may be ordered when clinically indicated.
Appendix A
Pathophysiology of uric acid calculi and associated conditions.
| Low urine pH |
| Obesity |
| Type II diabetes mellitus |
| Metabolic syndrome |
| Chronic diarrhea |
| Primary gout |
| Excess animal protein |
| Hyperuricosuria |
| Uricosuric medications |
| Congenital disorders |
| Myeloproliferative disorders |
| Primary gout |
| Excess animal protein |
| Low urine volume |
| Inadequate fluid intake |
| Chronic diarrhea |
Appendix B
Management of uric acid calculi by specific urinary abnormalities
| Urinary Abnormality | Treatment | Mechanism of Action | Adult
Dosage |
Adverse Effects | Monitor |
| Low urine pH | Potassium citrate | Provides alkali load that increases urine pH | 40-60 mEq/day, titrate to desired pH | GI side effects | Urine pH, serum electrolytes, BUN, creatinine |
| Profound Hyperuricosuria | Allopurinol
Febuxostat |
Xanthine oxidase inhibitor that reduces serum and urinary uric acid | 100-300 mg/day | Elevated transaminases, Stevens-Johnson syndrome, xanthinuria | Serum uric acid and liver enzymes |
| Low urine volume | Increase fluid intake | Increase urine volume | Urine output of 2.5 L/day | N/A | N/A |
References
Shattock JG. A prehistoric or predynastic Egyptian calculus. Trans Path Soc Lon 1905; 61: 275
Scales CD, Jr, Smith AC, Hanley JM, Saigal CS Urologic Diseases in America Project, authors. Prevalence of kidney stones in the United States. Eur Urol. 2012;62:160–165.
Balinsky JB. Phylogenetic aspects of purine metabolism. S Afr Med J. 1972;46(29):993–7.
Campbell JW. Comparative biochemistry of nitrogen metabolism. In: Campbell JW, editor. The vertebrates. Vol. 2. New York: Academic Press; 1970.
DELETED
Pak CY, et al. Physicochemical metabolic characteristics for calcium oxalate stone formation in patients with gouty diathesis. J Urol. 2005;173(5):1606–9.
Pak CY, et al. Biochemical distinction between hyperuricosuric calcium urolithiasis and gouty diathesis. Urology. 2002;60(5):789–94.
Pak CY, et al. Biochemical profile of idiopathic uric acid nephrolithiasis. Kidney Int. 2001;60(2):757–61.
Sakhaee K, et al. Pathophysiologic basis for normouricosuric uric acid nephrolithiasis. Kidney Int. 2002;62(3):971–9.
Abate N, Chandalia M, Cabo-Chan AV, Moe OW, Sakhaee K. The metabolic syndrome and uric acid nephrolithiasis: novel features of renal manifestation of insulin resistance. Kidney Int. 2004;65:386–392.
Maalouf NM, Cameron MA, Moe OW, Adams-Huet B, Sakhaee K. Low urine pH: a novel feature of the metabolic syndrome. Clin J Am Soc Nephrol. 2007;2:883–888.
Taylor EN, Stampfer MJ, Curhan GC. Obesity, weight gain, and the risk of kidney stones. JAMA. 2005;293:455–462.
Moe OW. Kidney stones: pathophysiology and medical management. Lancet. 2006;367:333-344.
Stamatelou KK, Francis ME, Jones CA, et al. Time trends in reported prevalence of kidney stones in the United States: 1976-1994. Kidney Int. 2003;63:1817-1823.
Gutman AB, Yu TF. Uric acid nephrolithiasis. Am J Med. 1968;45:756–779.
Mandel NS, Mandel GS. Urinary tract stone disease in the United States veteran population. I. Geographical frequency of occurrence. J Urol. 1989;142:1513–1515.
Mandel NS, Mandel GS. Urinary tract stone disease in the United States veteran population. II. Geographical analysis of variations in composition. J Urol. 1989;142:1516–1521.
Gault MH, Chafe L. Relationship of frequency, age, sex, stone weight, and composition in 15,624 stones: comparison of results for 1980 to 1983 and 1995 to 1998. J Urol. 2000;164:302–307.
Lieske JC, Rule AD, Krambeck AE, Williams JC, Bergstralh EJ, Mehta RA, Moyer TP. Stone composition as a function of age and sex. Clin J Am Soc Nephrol. 2014;9(12):2141–6.
Gentle DL, Stoller ML, Bruce JE, Leslie SW. Geriatric urolithiasis. J Urol. 1997;158:2221–2224.
Rafique M, Bhutta RA, Rauf A, Chaudhry IA. Chemical composition of upper renal tract calculi in Multan. J Pak Med Assoc. 2000 May;50(5):145–8.
Herbstein FH, Kleeberg J, Shalitin Y, Wartski E, Wielinski S. Chemical and x-ray diffraction analysis of urinary stones in Israel. Isr J Med Sci. 1974 Dec;10(12):1493–9.
Hossain RZ, Ogawa Y, Hokama S, Morozumi M, Hatano T. Urolithiasis in Okinawa, Japan: a relatively high prevalence of uric acid stones. Int J Urol. 2003 Aug;10(8):411–5.
Pak CY, Sakhaee K, Moe O, Preminger GM, Poindexter JR, Peterson RD, Pietrow P, Ekeruo W. Biochemical profile of stone-forming patients with diabetes mellitus. Urology. 2003 Mar;61(3):523–7.
Daudon M, Lacour B, Jungers P. High prevalence of uric acid calculi in diabetic stone formers. Nephrol Dial Transplant. 2005 Feb;20(2):468–9.
Cameron MA, Maalouf NM, Adams-Huet B, Moe OW, Sakhaee K. Urine composition in type 2 diabetes: predisposition to uric acid nephrolithiasis. J Am Soc Nephrol. 2006 May;17(5):1422–8.
Lieske JC, de la Vega LS, Gettman MT, Slezak JM, Bergstralh EJ, Melton LJ, 3rd, Leibson CL. Diabetes mellitus and the risk of urinary tract stones: a population-based case-control study. Am J Kidney Dis. 2006 Dec;48(6):897–904.
Ekeruo WO, Tan YH, Young MD, Dahm P, Maloney ME, Mathias BJ, Albala DM, Preminger GM. Metabolic risk factors and the impact of medical therapy on the management of nephrolithiasis in obese patients. J Urol. 2004 Jul;172(1):159–63.
Daudon M, Lacour B, Jungers P. Influence of body size on urinary stone composition in men and women. Urol Res. 2006 Jun;34(3):193–9.
Daudon M, Traxer O, Conort P, Lacour B, Jungers P. Type 2 diabetes increases the risk for uric acid stones. J Am Soc Nephrol. 2006 Jul;17(7):2026–33.
Oda M, Satta Y, Takenaka O, Takahata N. Loss of urate oxidase activity in hominoids and its evolutionary implications. Mol Biol Evol. 2002;19:640–653.
Anzai N, Enomoto A, Endou H. Renal urate handling: clinical relevance of recent advances. Curr Rheumatol Rep. 2005;7:227–234.
Gutman AB, Yu TF. A three-component system for renal excretion of uric acid in man. Trans Assoc Am Physicians. 1961;74:353–365.
Steele TH, Boner G. Origins of the uricosuric response. J Clin Invest. 1973;52:1368–1375.
Enomoto A, Kimura H, Chairoungdua A, et al. Molecular identification of a renal urate anion exchanger that regulates blood urate levels. Nature. 2002;417:447–452.
Matsuo H, et al. ABCG2 dysfunction causes hyperuricemia due to both renal urate underexcretion and renal urate overload. Sci Rep. 2014;4:3755. doi: 10.1038/srep03755.
Maalouf NM, Cameron MA, Moe OW, Sakhaee K. Novel insights into the pathogenesis of uric acid nephrolithiasis. Curr Opin Nephrol Hypertens. 2004 Mar;13(2):181–9.
Finlayson B, Smith A. Stability of first dissociable proton of uric acid. J Chemical and Engineering Data1974 January. 1974;19(1):94–7.
Bobulescu IA, et al. Effect of renal lipid accumulation on proximal tubule Na+/H+ exchange and ammonium secretion. Am J Physiol Renal Physiol. 2008; 294(6):F1315–22. [PubMed: 18417539]
Bobulescu IA, et al. Reduction of renal triglyceride accumulation: effects on proximal tubule Na+/H+ exchange and urinary acidification. Am J Physiol Renal Physiol. 2009; 297(5):F1419–26. [PubMed: 19692486]
Maalouf NM, Sakhaee K, Parks JH, et al. Association of urinary pH with body weight in nephrolithiasis. Kidney Int. 2004;65:1422–1425.
Patel ND, Ward RD, Calle J, Remer EM, Monga M. Computerized Tomography Based Diagnosis of Visceral Obesity and Hepatic Steatosis is Associated with Low Urine pH. J Urol 2017; 198(5): 1085-10
Eisner BH, Porten SP, Bechis SK, Stoller ML. Diabetic kidney stone formers excrete more oxalate and have lower urine pH than nondiabetic stone formers. J Urol 2010; 183(6): 2244-8
Torricelli FC, De SK, Gebreselassie S, Li I, Sarkissian C, Monga M. Dyslipidemia and kidney stone risk. J Urol 2014 191(3): 667-72.
Torricelli FC, De S, Gebreselassie S, Li I, Sarkissian C, Monga M. Type-2 diabetes and kidney stones: impact of diabetes medications and glycemic control. Urology 2014; 84(3): 544-8.
Bobulescu IA and Moe OW: Renal transport of uric acid: evolving concepts and uncertainties. Adv Chronic Kidney Dis 2012; 19: 358.
Khatchadourian J, Preminger GM, Whitson PA, et al. Clinical and biochemical presentation of gouty diathesis: comparison of uric acid versus pure calcium stone formation. J Urol. 1995;154:1665–1669.
Zerwekh JE, Holt K, Pak CY. Natural urinary macromolecular inhibitors: attenuation of inhibitory activity by urate salts. Kidney Int. 1983;23:838–841.
Robertson WG. Renal stones in the tropics. Semin Nephrol. 2003;23:77–87.
el-Reshaid K, Mughal H, Kapoor M. Epidemiological profile, mineral metabolic pattern and crystallographic analysis of urolithiasis in Kuwait. Eur J Epidemiol. 1997;13:229–234.
Borghi L, Meschi T, Amato F, et al. Hot occupation and nephrolithiasis. J Urol. 1993;150:1757–1760.
Shekarriz B, Stoller ML. Uric acid nephrolithiasis: current concepts and controversies. J Urol. 2002;168:1307–1314.
Deren JJ, Porush JG, Levitt MF, Khilnani MT. Nephrolithiasis as a complication of ulcerative colitis and regional enteritis. Ann Intern Med. 1962 Jun;56:843–53.
Gelzayd EA, Breuer RI, Kirsner JB. Nephrolithiasis in inflammatory bowel disease. Am J Dig Dis. 1968 Dec;13(12):1027–34.
Knudsen L, Marcussen H, Fleckenstein P, Pedersen EB, Jarnum S. Urolithiasis in chronic inflammatory bowel disease. Scand J Gastroenterol. 1978;13(4):433–6.
Bambach CP, Robertson WG, Peacock M, Hill GL. Effect of intestinal surgery on the risk of urinary stone formation. Gut. 1981 Apr;22(4):257–63.
Fukushima T, Yamazaki Y, Sugita A, Tsuchiya S. Prophylaxis of uric acid stone in patients with inflammatory bowel disease following extensive colonic resection. Gastroenterol Jpn. 1991 Aug;26(4):430–4.
Clarke AM, McKenzie RG. Ileostomy and the risk of urinary uric acid stones. Lancet. 1969 Aug 23;2(7617):395–7.
Obialo CI, Clayman RV, Matts JP, Fitch LL, Buchwald H, Gillis M, Hruska KA. Pathogenesis of nephrolithiasis post-partial ileal bypass surgery: case-control study. The POSCH Group. Kidney Int. 1991 Jun;39(6):1249–54.
McLeod RS, Churchill DN. Urolithiasis complicating inflammatory bowel disease. J Urol. 1992;148:974–978.
Howard SC, Jones DP, Pui CH. The tumor lysis syndrome. N Engl J Med. 2011; 364(19):1844–54.
Low RK, Stoller ML. Uric acid-related nephrolithiasis. Urol Clin North Am. 1997;24:135–148.
Tsimberidou AM, Keating MJ. Hyperuricemic syndromes in cancer patients. Contrib Nephrol. 2005;147:47–60.
Wilson JM, Young AB, Kelley WN. Hypoxanthineguanine phosphoribosyltransferase deficiency. The molecular basis of the clinical syndromes. N Engl J Med. 1983;309:900–910.
Talente GM, Coleman RA, Alter C, et al. Glycogen storage disease in adults. Ann Intern Med. 1994;120:218–226.
Eskelinen M, Ikonen J, Lipponen P: Usefulness of history-taking, physical examination and diagnostic scoring in acute renal colic. Eur Urol 34: 467, 1998
Kadlec AO, Greco K, Fridirici ZC, Hart ST, Vellos T, Turk TM. Metabolic syndrome and urinary stone composition: what factors matter most? Urology 2012; 80(4): 805-10
Smith RC, Verga M, McCarthy S, Rosenfield AT. Diagnosis of acute flank pain: value of unenhanced helical CT. AJR Am J Roentgenol. 1996;166:97–101.
Dalrymple NC, Verga M, Anderson KR, et al. The value of unenhanced helical computerized tomography in the management of acute flank pain. J Urol. 1998;159:735–740.
Hidas et al, 2010. Hidas G, Eliahou R, Duvdevani M, et al: Determination of renal stone composition with dual-energy CT: in vivo analysis and comparison with x-ray diffraction. Radiology 2010; 257: pp. 394-401.
Ray AA, Ghiculete D, Pace KT, et al. Limitations to ultrasound in the detection and measurement of urinary tract calculi. Urology. 2010;76:295.
Graff L. A handbook of routine urinalysis. Philadelphia: J.B. Lippincott Company; 1982.
Wolf JS Jr, Bub WL, Endicott RC, Clayman RV. Use of intravenous contrast material during in situ extracorporeal shock wave lithotripsy of ureteral calculi. J Urol. 1997 Jan;157(1):38-41.
N. P. Buchholz, M. van Rossum. Shock wave lithotripsy treatment of radiolucent ureteric calculi with the help of contrast medium. Eur Urol. 2001 Feb; 39(2): 200–203.
Moran ME, Abrahams HM, Burday DE, Greene TD. Utility of oral dissolution therapy in the management of referred patients with secondarily treated uric acid stones. Urology. 2002 Feb; 59(2): 206–210.
Elderwy AA, Kurkar A, Hussein A, et al. Dissolution therapy versus shock wave lithotripsy for radiolucent renal stones in children: a prospective study. J Urol. 2014 May; 191(5 Suppl): 1491–1495.
Pak CY, Sakhaee K, Fuller C. Successful management of uric acid nephrolithiasis with potassium citrate. Kidney Int. 1986;30(3):422–8.
Preminger GM, Sakhaee K and Pak CY: Alkali action on the urinary crystallization of calcium salts: contrasting responses to sodium citrate and potassium citrate. J Urol 1988; 139: 240.
Sterrett SP, Penniston KL, Wolf JS Jr, et al. Acetazolamide is an effective adjunct for urinary alkalization in patients with uric acid and cystine stone formation recalcitrant to potassium citrate. Urology. 2008;72:278–81.
Wabner CL, Pak CY. Effect of orange juice consumption on urinary stone risk factors. J Urol. 1993;149:1405–1408.
Odvina CV. Comparative value of orange juice versus lemonade in reducing stone-forming risk. Clin J Am Soc Nephrol. 2006;1(6):1269–74.
N. A. Breslau, L. Brinkley, K. D. Hill, C. Y. Pak. Relationship of animal protein-rich diet to kidney stone formation and calcium metabolism. J Clin Endocrinol Metab. 1988 Jan; 66(1): 140–146.
Taylor EN, Fung TT, Curhan GC. DASH-style diet associates with reduced risk for kidney stones. J Am Soc Nephrol. 2009;20:2253–2259.
Taylor E.N., Stampfer M.J., Mount D.B., Curhan G.C. DASH-style diet and 24-hr urine composition. Clin. J. Am. Soc. Nephrol. 2010;5:2315–2322.
Pearle M. S., Goldfarb D. S., Assimos D. G., Curhan G., Denu‐Ciocca C. J., Matlaga B. R., et al. 2014. Medical management of kidney stones: AUA guideline. J. Urol. 192:316–324.
Study Questions
- A 56-year-old obese female with a history of insulin resistant diabetes mellitus presents to the emergency department with acute left-sided flank pain radiating towards her groin. Her pain is adequately controlled, and the appropriate treatment is started. 5 days later, she passes many small stones primarily composed of uric acid. What is the major factor in the pathogenesis of this condition?
- increased urinary uric acid
- low urinary pH
- low urine volume
- urinary stasis
- What is the proposed theory for persistently acidic urine in patients with insulin resistance and features of metabolic syndrome?
- increased proton pump activity in the collecting duct
- purine gluttony leading to increased urinary acid production
- lipotoxicity of the proximal tubule cells leading to defective ammonium generation
- increased urinary bicarbonate reabsorption
- A 45-year-old obese male presents to the emergency room with acute renal colic. Upon further questioning, he states that he has been adhering to a low-carb, high-protein diet. Urinalysis reveals a urine pH of 6.5 and microscopic hematuria. What is the most likely stone composition?
- mixed calcium oxalate and urate
- struvite
- hydroxyapatite
- uric acid
- A 54-year-old male presents to the emergency department with sudden-onset, excruciating right flank pain radiating to his groin. What is the imaging modality of choice when evaluating this patient?
- KUB
- ultrasound
- non-contrast CT scan
- MRI
- A 61-year-old man with insulin resistant diabetes mellitus and normal renal function presents to the urologist with recurrent uric acid stones. He wants to prevent further stones. The first line treatment is
- allopurinol
- sodium bicarbonate
- febuxostat
- potassium citrate
- A 48-year-old man with hyperuricosuric calcium oxalate stones presents to the urologist for follow-up. Since his last visit, he has reduced his animal protein intake in hopes of reducing urinary uric acid levels. Today, a 24-hour urinalysis shows hyperuricosuria and normocalciuria. What is the next best step in management?
- restrict dietary calcium intake
- allopurinol
- carbonic anhydrase inhibitors
- hydrochlorothiazide
- T/F Uric acid stones are easily visualized on KUB and therefore are amenable to shock wave lithotripsy treatment.
Answers
- B. An overly acidic urine is the most important factor in the pathogenesis of uric acid stone formation, as it lowers the solubility of uric acid to where even moderate amounts will precipitate and form a stone.
- C. Experiments with the Zucker rat, a model for metabolic syndrome showed that these animals have lower urine pH, lower urinary ammonium excretion and a higher net acid excretion as compared to lean rats. These differences may be related to an increase in renal fat deposition, with fat content being significantly higher in the Zucker rat kidneys.
- A. While patients with hyperuricosuria are at risk for uric acid stone disease, in the presence of a normal urinary pH, mixed calcium oxalate/urate are more likely. Pure uric acid stones are less likely, as low urinary pH is the main factor in uric acid precipitation.
- C. A non-contrast CT has the best sensitivity and specificity for kidney stone detection. Radiolucent stones (uric acid) do not appear on radiographs and a non-contrast CT can be used to differentiate between uric acid and calcium stones based on the low Hounsfield values (200-400) of uric acid stones.
- D. The first line treatment for uric acid stones is alkalization therapy with potassium citrate.
- B. Allopurinol is only indicated in uric acid stone formers who fail alkalization therapy or in calcium oxalate stone formers with hyperuricosuria and normocalciuria.
- 7. F. Uric acid stones often cannot be seen on KUB and have Hounsfield units of 300-400, and thus shock wave lithotripsy is often not used as a treatment option.
#dissertation #thesis #essay #assignment #phd #phdstudent #phdlife #essaywriting #research #phdjourney #dissertationlife #gradschool #assignments #phdproblems #academicwriting #assignmenthelp #thesiswriting #gradstudent #dissertationproblems #university #academiclife #gradschoolproblems #academia #researchpaper #gradschoollife #graduateschool #college #doctoralstudent #dissertationdone #writing